Introduction
The high dose rate prostatic brachytherapy program at the Wesley Hospital combines external beam radiation treatment with temporary transperineal insertion of brachytherapy needles directly into the prostate gland. Via these needles 3 fractions of high dose rate radiation treatment are delivered in 3 separate fractions, separated by a minimum of 6 hours.
Results of HDR brachytherapy at the Wesley Hospital
Wesley Hospital first commenced the HDR prostatic brachytherapy program in August 2000. By June, 2010 over 860 patients have been treated with HDR brachytherapy at the Wesley Hospital. Traditionally high dose rate brachytherapy has been used to treat patients with high risk prostate cancer. These patients usually have disease considered too advanced for surgical intervention, or alternatively patients have multiple intermediate risk factors and wish to avoid a radical prostatectomy procedure.
We reviewed the results of our first 350 patients with a minimum follow up of 4 years (median 6 years).
Outcome Statified by Risk – minimum 4 years follow up (median 6 years).
| Patient Type | Clinical Local Control | Biochemical freedom from disease (Astro definition) |
|---|---|---|
| High Risk – Stage T3a nodule, or PSA >20, or Gleason 8 – 10 tumour) | 97% | 77% |
| Intermittent Prostate Cancer – Palpable nodule stage T2,or Gleason 7 or PSA 10 – 20 | 99% | 91% |
Rationale for HDR brachytherapy
The total dose of external beam radiation therapy that can be delivered to the prostate, is limited by the tolerability of the surrounding structures to this radiation treatment. The bowel (rectum) and bladder are in close proximity to the prostate gland and do receive radiation dose during external beam radiation treatment. Once a certain dose of external beam radiation is delivered (usually 74Gy) then considerable side effects can occur including chronic bowel bleeding, pain, mucous production, rectal frequency and urgency, bladder irritability, blood in the urine, haematuria and urethral stricture. Rarely prostate-rectal fistula’s can occur requiring a colostomy, when very high doses of radiotherapy are used.
By inserting brachytherapy needles directly into the prostate the radiation dose can be delivered more accurately to the prostate gland, limiting the damage to structures around the prostate such as the bladder and rectum.
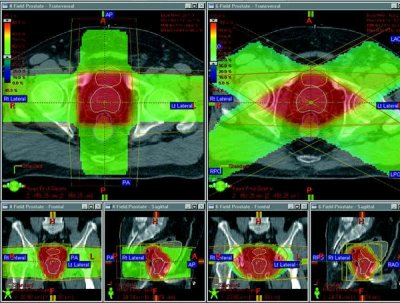
Figure 1 – External Beam Radiotherapy
This diagram shows the radiation dose to the surrounding structures with external beam radiotherapy. The green shaded areas are the external beam radiation dose delivered from the outside of the body into the prostate gland. The prostate is marked out in red.
Where all the green external beam radiation doses meet (the red shaded area) this is where the highest dose of radiotherapy therapy (100% dose) occurs. You can see from this drawing that the bladder and bowel are also affected with the radiation treatment.
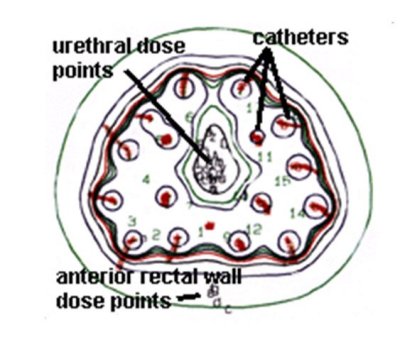
Figure 2 – Radiation figure
This figure shows the radiation dose delivered by the brachytherapy treatment to the prostate gland. As you can see the 100% dose is limited to just outside the prostate gland with rapid fall off of radiation dose as you more away from the brachytherapy needle. Therefore the anterior rectum receives much less radiotherapy (approximately 50%) compared with what would be delivered with external beam treatment. The posterior rectum receives almost no radiation treatment at all! Due to the accuracy of this treatment we can deliver potentially a higher dose of radiation to the prostate than would be achieved with external beam treatment. There is evidence to suggest that radiation dose escalation improves local control of prostate cancer and also long term “cure” or biochemical freedom from disease.
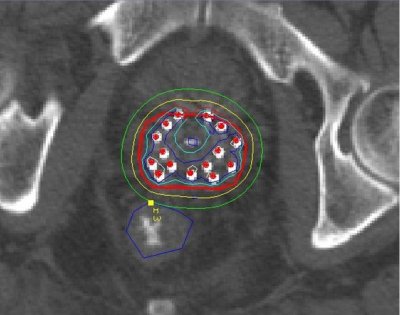
Figure 3 – CT Scan
This figure is a CT scan as shows the dosimetry achieved during high dose rate brachytherapy treatment. The prostate is again marked in red and the yellow line marks 100% dose line achieving a margin around the prostate gland to cover any microscopic extension of the tumour outside the prostate. However the amount of radiation touching the tip of the rectum is only 50% and almost no radiation affects the lower half of the rectum. Inside the prostate gland even higher doses are achieved (150-200% of the prescribed dose), particularly in areas where we know that the prostate cancer exists.
How are the HDR Brachytherapy needles inserted
The high dose brachytherapy needles are inserted in the operating theatre under a spinal general anaesthetic. Therefore this is a painless procedure. The needles are inserted through the skin (perineum) that lies between the testicles and anus. Usually 17 needles are inserted but the number may vary depending upon the size of the prostate gland and each individuals prostate anatomy. As a spinal anaesthetic is used during this procedure patients usually do not develop much pain over the first 12-24 hours although discomfort can occur on the first post operative day.
The brachytherapy needles are inserted in the operating theatre usually at approximately 8 o’clock in the morning and the patient then travels to the x-ray department for a CT scan to check the position of the needles. After the radiotherapists and radiation physicists calculate the appropriate dosimetry the first brachytherapy treatment is usually delivered at approximately 1500pm that day. The following day the patient receives two further fractions of radiation treatment at approximately 0800am and 1500pm. After the third dose the brachytherapy needles are removed. Therefore the needles only remain for one night.
The brachytherapy treatment is usually combined with a course of external beam radiotherapy. However the external beam dose is decreased to 46Gy which again decreases the “damage” to surrounding structures.
When combining the 46Gy of external beam radiotherapy with the HDR brachytherapy treatment, the radiobiological dose equivalent is at least 86Gy which is a higher dose then what would safely be able to be delivered by external beam radiation therapy alone. This therefore offers the potential for improved long term local control and biochemical freedom from disease.
Complications of HDR Brachytherapy
High dose rate brachytherapy is generally a well tolerated treatment. The recovery rate is fast and the patients are usually back at work within one week of the brachytherapy treatment.
The main complications of HDR brachytherapy are as follows, but no limited to,
- Urinary Frequency:
- It is very common to have urinary frequency and urgency of urination in the early post implant period. These symptoms usually recover from the first three months after treatment. The chance of having persisting bothersome voiding symptoms more then one year post treatment is < 10%.
- Rectal Discomfort:
- There is a dose of radiotherapy delivered to the rectum and therefore symptoms such as a more loose bowel motion, frequency of bowel movements and occasionally bleeding can occur. It is rare that these symptoms are a permanent. With external beam therapy the prevalence of grade 2 rectal toxicity in the RTOG studies in Australasia is 20%. The incidence of grade 2 toxicity in HDR brachytherapy is <5%.
- Urethral Stricture:
- The high doses of radiotherapy can occasionally scar the urethral tube as it exists through the prostate into the penile urethra. The risks of severe scarring requiring surgical intervention is approximately 5 – 10%. In these circumstances patients will require an operation to “dilate” the narrowing of the urethral tube. It may also be necessary for patients to perform intermittent catheterisation of their urethral tube to prevent recurrent scarring.
- Impotence:
- Over a five year period approximately 50% of patients who have been sexually active pre-operatively will lose their erections. Treatment such as oral tablets with Viagra may help.
- Bleeding:
- Blood in the urine can occur in the post implantation period, particularly in the first 24 hours following removal of the brachytherapy needles. Long term bleeding is uncommon.
- Penile Numbness:
- We have had four patients in our first 450 who have described numbness of the penis. This will usually resolve within the first 12 months.
- Rectal Bleeding or Pain:
- Early bleeding or mucous production is not uncommon but long term bleeding requiring intervention or medication occurs in <5% of patients.
- Prostato-Rectal Fistula:
- This is a rare complicaton of brachytherapy requiring a colostomy. No patient at the Wesley Hospital has developed this complication. Biopsies of the rectal wall during a colonoscopy or TRUS biopsies after HDR brachytherapy is to be avoided.

